Patient-Centered Medical Home Definition And Requirements
OHIC’s affordability initiatives have emphasized the need for a strong primary care infrastructure and since 2011, OHIC has been promoting PCMH transformation to help strengthen Rhode Island’s primary care network. In 2015, OHIC worked with its Care Transformation Advisory Committee to define patient-centered medical homes and to set a year over year insurer target for PCMH adoption. OHIC also requires that insurers make supplemental payments to designated primary care practices recognized by OHIC as PCMHs to help finance PCMH transformation and operations.
The three-part definition of a PCMH requires demonstration of practice transformation, implementation of cost management initiatives, and clinical quality performance attainment or improvement. This three-part definition of PCMH also includes a provider reporting component.
Note: All practices are required to submit basic information about their practice, indicate their Practice Transformation status, and answer the Behavioral Health Integration survey questions. Only practices not participating in at least one commercial Accountable Care Organization (ACO) population-based contract and not part of an FQHC-based Accountable Entity (AE) are required to complete the PCMH Quality Measures and Cost Management components of the surveys.
Definition of Patient-Centered Medical Home:
OHIC's 2020 regulations outline the following three-part definition of PCMH against which RI primary care practices will be evaluated:
- Practice is recognized by CTC-RI, participating for the first time in a formal transformation initiative and/or practice is recognized by a national accreditation body (e.g., NCQA recognition). Practices meeting this requirement through achievement of NCQA recognition may do so independent of participating in a formal transformation initiative.
- Practice has demonstrated clinical quality performance attainment or improvement. To promote measure alignment across statewide initiatives, measures selected to measure performance improvement will be selected from the OHIC multi-payer aligned measure set.
- Practice has implemented a quality improvement strategy targeted at cost management. Beginning in 2022, OHIC has waived this requirement for ACO-affiliated practices. Non-ACO-affiliated practices will need to separately implement one of OHIC's approved quality improvement strategies care coordination or cost-effective use of services to meet this requirement. These practices will be evaluated based on responses to an OHIC-administered survey.
Measures Included in the 2025 PCMH Measure Set
- In 2025, practices will need to report on the following measures for the 1/1/2025 - 12/31/2025 measurement period.
Adult practices
- Colorectal Cancer Screening (NCQA HEDIS, modified by CTC-RI)
- Eye Exam for Patients with Diabetes (NCQA HEDIS, modified by CTC-RI)
- Glycemic Status Assessment for Patients with Diabetes (<8.0%) (NCQA HEDIS, modified by CTC-RI)*
- Controlling High Blood Pressure (NCQA HEDIS, modified by CTC-RI)
*This measure has undergone significant specification changes for 2024 and will remain as a reporting-only for 2025.
Pediatric practices
- Child and Adolescent Well-Care Visits (12 - 17) (NCQA HEDIS, modified by CTC-RI)
- Developmental Screening in the First Three Years of Life (OHSU, modified by CTC-RI)
- Lead Screening in Children (NCQA HEDIS, modified by RIDOH to define the attributed population)**
**Pediatric practices will not need to submit data to OHIC for “Lead Screening in Children”. With practice permission, RIDOH will provide OHIC with practice reports for performance for the 1/1/2025 - 12/31/2025 measurement year for this measure. OHIC will share these final performance data with practices once it receives data from RIDOH’s KIDSNET. Practices can log onto KIDSNET on that date, or at any other time, to estimate performance on the measure.
Detailed specifications for these measures can be found in the following PDF:
A practice seeking OHIC PCMH recognition status is required to demonstrate attainment or improvement by reporting:
- practice performance at or above a pre-defined high-performance benchmark or
- improvement of at least three percentage points over one or two years.
Please note that 2023, OHIC reinstated the methodology for assessing practice performance against the PCMH Measure Set, which was not in place during the 2020-2021 and 2021-2022 PCMH assessments due to the impact of COVID-19 on quality measure performance. Practices must meet a high-performance benchmark or demonstrate three percentage-point improvement over the October 1, 2022 – September 30, 2023 performance period or the October 1, 2023 - September 30, 2024 performance period.
Adult practices need to demonstrate attainment or improvement on at least two of the three adult measures. Pediatric practices need to demonstrate attainment or improvement on at least two of the three pediatric measures. Practices that report on both adult and pediatric measures need to demonstrate attainment or improvement on at least two of the three adult measures and two of the three pediatric measures.
Similar to prior years, practices reporting for the first time in 2025 will not be assessed by demonstrating attainment or improvement. Instead, practices will meet the requirement simply by reporting performance on these measures. Performance will be recorded as baseline data and will be utilized to assess performance improvement in future years.
The high-performance benchmarks for 2025 reporting are as follows:
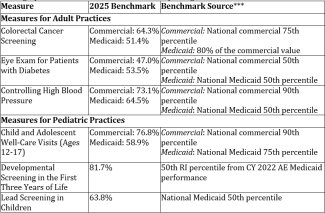
***HEDIS national data are from NCQA’s Quality Compass 2024 (CY 2023 data).
Additionally, when assessing if a practice demonstrated improvement, OHIC excludes rates with a denominator of less than 30 and rates submitted for a performance period other than what is indicated. OHIC, however, makes one-time exceptions to this methodology when measures move from reporting-only status to recognition status. OHIC also excludes these rates when calculating statewide median performance. It does not exclude these rates when assessing practice performance against the high-performance benchmark.
For more information or if you have any questions, please Charles Estabrook, Director of Policy, at charles.estabrook@ohic.ri.gov
Once the survey information has been collected and analyzed, OHIC will post on its website a list of practices and which elements of the PCMH definition they have met.
2025 Performance Improvement Survey
For more information or if you have any questions, please contact Charles Estabrook, Director of Policy, at charles.estabrook@ohic.ri.gov
